The subject of prenatal tests often evokes many emotions in parents-to-be – it brings joy and a feeling of relief when the results are correct (i.e. the risk of genetic abnormalities is low), and on the other hand, anxiety and fear when it turns out that the results are not correct.

Katarzyna Mikołajczyk, MD-PhD: There are times when a parent is left alone with the test results, where a row of numbers and graphs that tell them little cause unnecessary anxiety and stress. How to read the results of genetic prenatal tests?
Each time the result of a genetic test (whether non-invasive or invasive one) should be discussed with a specialist gynaecologist-obstetrician or geneticist, so that the patient receives full and factual information about the result, and has the opportunity to ask any questions that bother them.
This article will discuss how to interpret the results of screening tests, i.e., non-invasive tests that are performed in obstetric offices.
The first and most important thing – the result the patient receives is a risk, not the final diagnosis. Equally important, each test has a specific sensitivity and specificity, i.e. there are false positives (i.e. where the result is abnormal and the baby is healthy) and unfortunately negative results (where the test result is normal and a new-born is born ill).
The tests available at Medfemina Health Centre have the following sensitivity: ultrasound examination between 11-14 weeks of pregnancy according to FMF – 80%, combined test (ultrasound and double test) 92% and NIPT (examination of free foetal DNA) 99%. … The higher the sensitivity and specificity of the test, the lower the percentage of false-positive and negative results, i.e. the more precise the test.
ULTRASOUND IN 11-14 weeks of pregnancy and PAPP-A test
ULTRASOUND IN 11-14 weeks of pregnancy and PAPP-A test
The test result is presented as follows:
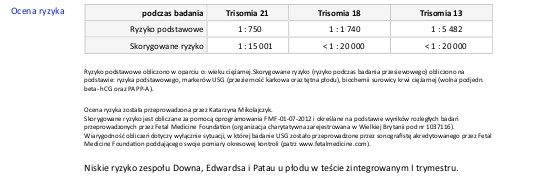
The resulting risk should be interpreted as follows:
The basic age-related risk of having a child with Down’s syndrome is 1: 750. After the ultrasound examination and in this case the double test (PAPP-A test), this risk drops to 1: 15001, which should be interpreted as follows: 1 in 15,001 women my age with results like mine will have a child with Down’s syndrome, the remaining 15,000 will be healthy; less than 1 woman in 20,000 with these results will have a child with Edwards / Patau syndrome, the remainder being healthy. Overall, the risk of chromosomal abnormalities in this particular pregnant woman is very low.
The risk higher than the population risk, i.e. higher than 1: 250-300, was assumed as high risk. In such a situation, the patient should consult a geneticist in order to consider diagnostic tests, mainly invasive, such as amniocentesis or trophoblast biopsy; only they will allow 100% diagnosis or exclusion of the disease in the foetus. When deciding to perform invasive tests, one should also take into account their risk – i.e. the risk of pregnancy loss, which is 0.5-1%.
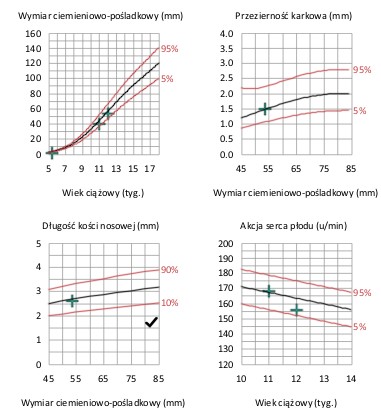
In addition to the risk, the patient is provided with graphs of the basic parameters assessed by ultrasound – the key risk factor is the nuchal fold (NT), which is the accumulation of fluid in the subcutaneous tissue of the foetus at the nape of the neck – an abnormal result is a nuchal fold width above the 95th percentile for a given foetal size (i.e., foetal crown-rump length (CRL) )- hence there is no single universal standard. And so, a neck fold of 2.5 mm in thickness for a foetus with a CRL 45 mm in length will be an abnormal result (above the 95th percentile), while for a foetus with a length of 80 mm – it will be a normal result. It should be remembered that dilated NT occurs not only in genetic defects, but also in some heart defects, infections, and sometimes also in healthy foetuses. Each dilated NT should be verified by diagnostic examination in terms of genetic defects and by ECHO (echocardiography), (ultrasound) of the foetal heart.
The next parameter to be assessed is the nasal bone, or rather its degree of ossification. Sometimes the patient gets the result „no nasal bone”. In fact, this means that these bones exist but ossify later and are therefore invisible or less visible on ultrasound. The nasal bone should be thicker and more visible than the outline of the skin of the nose, its length is of secondary importance. Such delayed ossification of the nasal bone is characteristic of, for example, Down’s syndrome and other genetic defects, but it can also occur in 1-3% of healthy children.
Assessment of the foetal heart rate: in period between 11th – 14th week of pregnancy, the foetal heart rate is approximately 155-170 beats per minute. Characteristically elevated / lowered foetal heart rates are found in specific genetic abnormalities (although in foetuses with Down syndrome the heart rate is usually normal). Other factors may also influence the foetal heart rate – mother’s additional diseases, infections, stress.
An important element of the first trimester ultrasound examination is also the assessment of the foetal anatomy in terms of major defects, as more than 60% of defects found in the foetus are developmental defects, not necessarily of genetic origin, while Down’s syndrome accounts for only 15% of all defects.
FREE FOETAL DNA TESTS
How to read the NIFTY test result? How do I read my Harmony test result?
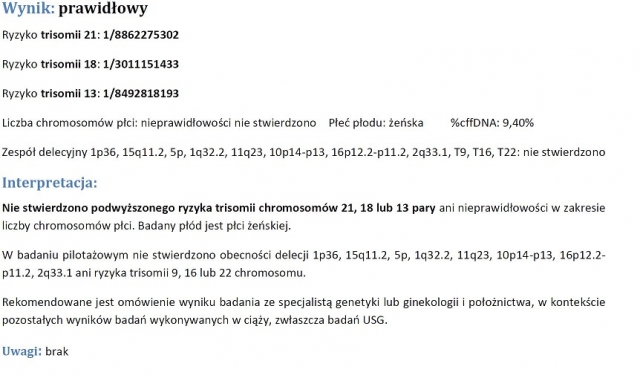
- An example of a correct result for free foetal DNA (NIFTY, HARMONY)
- Example of an abnormal free foetal DNA test result (NIFTY, HARMONY)

Although the free foetal DNA is properly tested, the result is also a risk, as indicated by the methodology of the test. Each time the test is accompanied by a comment whether the risk is high or low and what is the sensitivity of the method in a specific case. In the event of a high risk of a genetic defect in the foetus, a geneticist should be consulted as in the case of the tests described above. High risk is still not a final diagnosis. Only direct examination (from amniotic fluid, chorionic villus sampling) enables the final diagnosis to be made.
Due to the fact that non-invasive tests are associated with the risk of false results – both false positive and negative, each result should be interpreted comprehensively, analysing the result of an ultrasound examination, blood test, family history, hence the necessary consultation and discussion of the result with an obstetrician experienced in prenatal diagnostics or a geneticist.




 Registration from 8:00 am to 9:00 pm
Registration from 8:00 am to 9:00 pm On-line registration 24/7
On-line registration 24/7